Beyond the EAP: why workplace behaviour beats “programmes” for mental health (and performance)
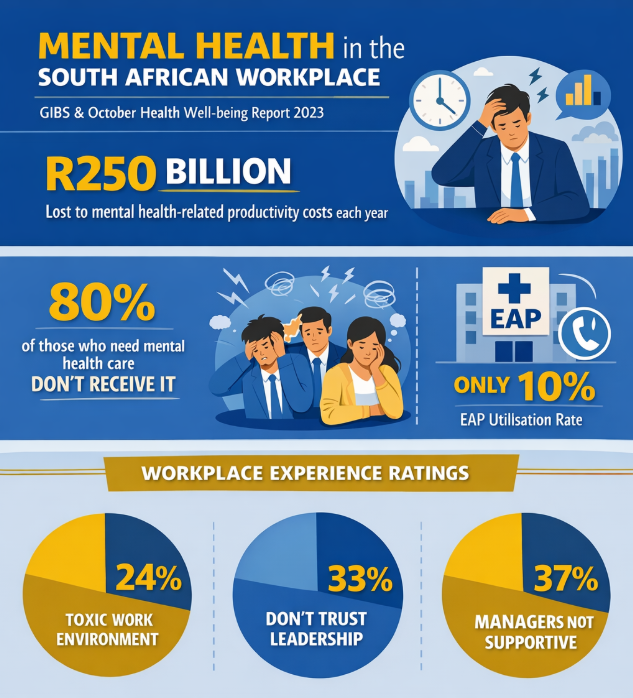
“An estimated 80% of people who need mental health care do not get it.” (GIBS) The GIBS x October Health Workplace Well-being Report points to a hard economic reality: mental health challenges are estimated to cost South Africa about R250 billion a year in lost productivity (largely from absenteeism and presenteeism), with knock-on effects on GDP.
That’s the macro story. The micro story is what your people experience every day: the tone of a manager’s feedback, whether mistakes are punished or learned from, whether work is fair, whether roles are clear, and whether teams feel like teams—or like competitors.
And that’s the shift many organisations need to make:
From “mental health support as a programme” → to “wellbeing as a behavioural and cultural system.”
The “scale” is the point: we can’t improve what we don’t measure
One of the most useful contributions from GIBS (in partnership with October Health) is that they’ve pushed workplace wellbeing into measurement, not just feeling.
Their Workplace Well-being Index and annual reporting set a baseline for how working South Africans are doing, and what factors influence that wellbeing. In other words: it’s not just how stressed people feel, it’s what’s driving it inside the workplace. (Bizcommunity)
That matters because most companies are still trying to solve wellbeing with disconnected efforts:
- an EAP
- a once-off wellness day
- a poster campaign
- an expensive leadership programme
None of these are inherently bad. But on their own, they’re rarely strong enough to change people’s day-to-day experience of work.
Mental health vs mental illness: why the distinction changes how leaders respond
A big reason workplace wellbeing conversations go nowhere is that we mix up mental health and mental illness.
- Mental health is a state of mental wellbeing, the ability to cope with normal stresses, learn and work well, and contribute to community. (World Health Organization)
- Mental illness refers to diagnosable conditions (for example major depressive disorder, anxiety disorders, substance use disorders, PTSD, etc.) that often require clinical care.
- Between those two is what many people experience at work: mental ill-health: high stress, low mood, burnout risk, overwhelm, or emotional fatigue that may not be a diagnosis, but absolutely affects performance and relationships.
Why does this matter? Because leaders often react in extremes:
- “This is HR’s problem.”
- “This person needs therapy.”
- “They must toughen up.”
Whereas the better approach is:
“What is the workplace environment doing to people’s state of mind, and what can we change in our behaviours, expectations, and workplace ecosystem?”
The EAP problem: it’s reactive, and people don’t use it
EAPs have a place. But they aren’t a wellbeing strategy.
A consistent theme in EAP research and practice is low utilisation, often in the single digits globally, with “strong engagement” sometimes described as closer to 7–10%. (EAPASA)
This aligns with what many organisations experience:
- people don’t know what’s available
- they don’t trust confidentiality
- they don’t want the stigma
- they only seek help when things have already escalated
And, critically, EAPs do not change the workplace behaviours that created the problem in the first place. So yes, keep the EAP. But stop pretending it’s the remedy.
What actually moves wellbeing? Daily behaviour and culture
The GIBS report explicitly points to the role of leadership and organisational culture in shaping employees’ mental and emotional state, and highlights concepts like psychological safety as a key enabler of wellbeing and performance.
This is where “behaviour in the workplace” becomes the real intervention.
Because people don’t experience culture as a slogan. They experience it as:
- how decisions are communicated
- how conflict is handled
- whether accountability is fair or political
- whether workloads are realistic
- whether feedback is respectful
- whether managers notice warning signs early
- whether teams collaborate or compete internally
Put simply:
Workplace wellbeing is built (or broken) in the moments between people.
“Flip the switch”: from mental health as crisis management to mental fitness for performance
If we want a practical way forward, we need to treat wellbeing like we treat performance:
Build capability. Build habits. Build capacity.
This is where performance psychology and “mental fitness” thinking becomes useful at work. Not in a fluffy way but in an operational way.
Examples of mental fitness tools that can be built into everyday work:
- stress regulation and recovery habits (micro-recovery, boundaries, workload planning)
- reframing and problem-solving under pressure
- emotional self-management in conflict
- role clarity conversations (so people aren’t living in endless ambiguity)
- team norms that prevent unnecessary friction (how we disagree, decide, escalate, and support)
The goal isn’t to turn managers into therapists. It’s to build leaders you can trust; leaders who can balance delivery with dignity.
Why this is also a Decent Work issue (SDGs + leadership responsibility)
If you link this to the Sustainable Development Goals, workplace wellbeing isn’t just an HR trend, it’s part of what quality work should look like.
- SDG 8 commits to “full and productive employment and decent work for all.” (Sustainable Development Goals)
- The ILO definition of decent work includes productive work in conditions of freedom, equity, security, and human dignity. (International Labour Organization)
A workplace that normalises fear, disrespect, constant overload, or internal competition at all costs is not “decent work”, even if it has an EAP and a fancy leadership programme.
Decent work shows up when people can perform and remain well enough to sustain that performance.
A practical starting point: what to do in the next 90 days
If you want to move beyond wellbeing as a tick-box, start here:
-
Measure your current state
Use a baseline assessment (wellbeing, psychological safety, workload, role clarity, team climate). Don’t start with solutions before you understand the situation. -
Identify the behaviour hotspots
Where is wellbeing breaking down? (Certain teams, managers, shifts, job families, or pressure points in the operating rhythm.) -
Equip leaders with a small set of non-negotiable behaviours
Not company values posters, rather observable behaviours (how feedback is given, how priorities are set, how work is planned, how mistakes are handled, how conflict is resolved). -
Build team norms that reduce friction
“Work as a team, not as competitors” needs a practical rule-set: decision rights, escalation paths, meeting discipline, and collaboration standards. -
Make support pathways visible and trusted
Your EAP (or other support) should be clear, easy, and stigma-free. But treat it as support, not the whole strategy. -
Track improvement quarterly
Tie wellbeing to performance indicators that matter: absenteeism, presenteeism signals, turnover risk, incident rates, rework, quality, engagement, and manager effectiveness
Where we’re headed
This is exactly why we’re intentionally moving further into wellbeing and organisational culture development advisory and consulting.
Because the real lever isn’t a “cookie cutter” programme.
It’s building workplaces where:
- leaders are trusted
- expectations are clear
- people can raise problems early
- teams collaborate properly
- performance is sustainable
Get a quick look at how you fair on our free human development assessment.